This quarter, I had the honor of speaking with Matthew MacDonald, M.D., a current third-year UCR family medicine resident (PGY-3). He is a 2013 La Sierra University alumnus and 2018 Loma Linda University School of Medicine graduate.
Like many La Sierra University students, Dr. MacDonald grew up in the “Jewel of the Inland Empire”: historic Redlands, radiating with sunshine over the fragrant orange groves. His medical journey began in high school while he participated in a research project with a neurosurgeon at Loma Linda University. At that stage in his life, he knew he wanted to pursue medicine as his calling because he loved learning about the anatomy and physiology of the human body (his favorite subject!). Moreover, biology fascinated his young mind. When rounding with the neurosurgeon, Dr. MacDonald was greatly inspired by the profound ability to apply a deep passion for the art of medicine and biology to not only help patients but also save lives. From that point forward, he continued to embark on the arduous expedition to earning his M.D. degree.
At La Sierra, Dr. MacDonald enrolled as a biology/pre-med major. Throughout his time at the university, he was very involved in on- and off-campus activities such as the Honors Program, Pre-Medical Society, research in the biology department, and volunteering. Albeit the stepping stones to medical school require much dedication to the stringent academic courses and commitment to community service, he was able to find a balance and have some fun in his life as well. He happily shared that some of his most memorable undergrad experiences include meeting his future wife in Honors, traveling on the “best trip of [his] life” to a one-month international adventure in Istanbul, Turkey, and learning from the best professors like Dr. Lee Grismer, Dr. Natasha Dean, and Dr. Eugene Joseph. Additionally, he cheerfully recalled fond memories of residing in South Hall as a “terrible prankster” with one of his friends. After four amazing college years, he graduated in 2013 from La Sierra University and was accepted into Loma Linda University School of Medicine’s Class of 2018.
Currently, Dr. MacDonald trains at the UCR Family Medicine Residency Program. He selected family medicine because he “wanted to do a bit of everything” and work with diverse patient populations at the opposite ends of the age spectrum –– pediatrics and adult patients. In his residency program, he rotates through various hospitals and clinics (i.e., St. Bernardine Medical Center, clinics in Banning and Temecula), where life can prove to be unpredictable. With that being said, there is not a fixed day in the life for a PGY-3 since the schedule changes on a monthly basis. At times, he may find himself working between 50 to 80 hours per week. During these erratic work shifts, he normally sees whatever comes in through the double doors but commonly treats the “bread and butter cases” –– gastrointestinal bleeds, heart attacks, chest pain, chronic obstructive pulmonary disease (COPD), asthma exacerbations, bronchiolitis, croup, appendicitis, colitis, drug abuse (hypertensive emergencies due to drugs like methamphetamines), and chronic health problems –– that family medicine doctors-in-training need to know, recognize, evaluate, diagnose, and treat. One of the most unusual cases in his medical career thus far has been a male patient who presented with a 12-inch foreign object lodged in his rectum.
Although it may seem that Dr. MacDonald has achieved the prestigious Grey’s Anatomy lifestyle like Meredith Grey and Cristina Yang, the reality of life as a physician is definitely not as glamorous as portrayed in popular culture by Shonda Rhimes, the creator of the medical drama series, now in its 17th year. The road to medicine is a very long yet worthwhile trip, but many doctors tend to undergo burnout and impostor syndrome throughout their medical training. Dr. MacDonald mentioned that it was “hard not to get burned out” as an intern, considering he spent “months on end working 80 hours per week.” However, he dealt with this universal condition by trying to relax, spending time with the people he loves, and having a strong therapeutic network to cushion against stress. He further explained that physical and emotional exhaustion may be overwhelming struggles for residents who live alone or do not have many family members and friends nearby. Thus, the physician suicide rate is very high, and the Accreditation Council for Graduate Medical Education (ACGME) has attempted to decrease these alarming numbers by implementing physician wellness programs. Nevertheless, Dr. MacDonald heavily emphasized that “social support makes a positive difference” in avoiding/minimizing the potentially fatal consequences of fatigue after long work hours.
On another note, those strenuous 80 hour work weeks can drastically interfere with the ideal work-life balance. Dr. MacDonald is still aiming to find that quintessential stability and maintain the mindset of just “trying to survive that month.” He strives to find the time to exercise to stay healthy, have dinner with his wife, and spend quality time with his family plus his three dogs (two Shih Tzus and a German Shepherd).
Over the past year, the COVID-19 pandemic has gravely taken the world by storm and claimed over 500,000 lives in the United States. Because of the strict social distancing guidelines and months of lockdowns, the life people once knew and took for granted was lugubriously affected. This includes the work and family life of physicians. The state’s devastating public health crisis significantly altered Dr. MacDonald’s residency training as hospital services became flooded, hours grew worse, and numerous difficult patients inundated the medical center floors. Residents need to see a particular number of cases before graduation, but the pandemic has limited the types of cases that could be seen. In the clinics, Dr. MacDonald now uses telemedicine technology to conduct virtual patient visits to ensure medically necessary services while mitigating the spreading of COVID-19 and its evolving variants. He frequently calls patients via Zoom or Doximity, a platform that enables doctors to directly contact patients from their personal phones and blocks physician phone numbers for privacy.
Despite all these obstacles in the new normal, physicians previously faced countless challenges even before the coronavirus outbreak. In medical school, third-year and fourth-year medical students (MS3s and MS4s) go through elective and core clinical rotations in specialties such as surgery, psychiatry, and internal medicine. Physicians-in-training can then integrate those valuable clinical clerkships in residency and as an attending. Dr. MacDonald described his intern year as having “a very steep learning curve.” While he had the knowledge of how to treat patients, he was applying these skills by himself for the first time and was “learning how to practice medicine.”
It is no secret that medical school is not without trials and tribulations. As a med student not too long ago, Dr. MacDonald mentioned that the greatest hurdle of all was “trying to survive medical school” since it was a “super stressful experience.” He elaborated that exams were around every possible corner, with major tests (comprehensive for every subject) given every three to four weeks. Furthermore, he cautioned that “you’re just always working towards the next thing.”
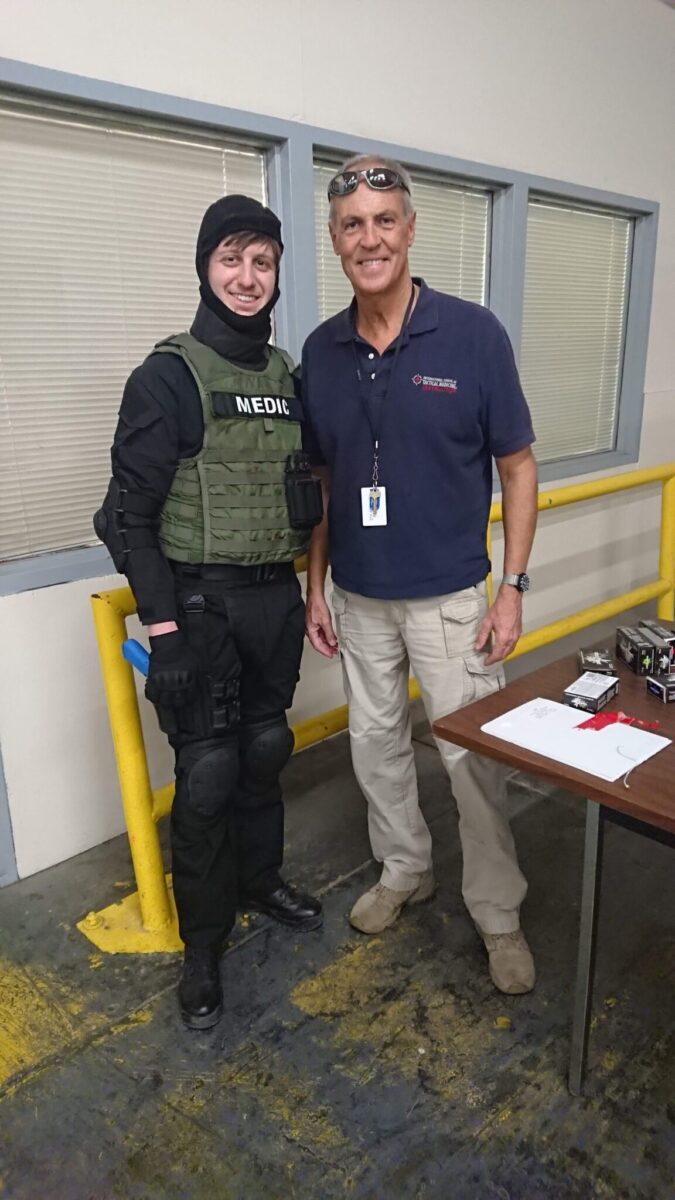
But, voilà! Dr. MacDonald accomplished every pre-med’s dream. A Redlands native, he attended La Sierra University, received medical training at Loma Linda University School of Medicine –– the dream institution for many La Sierra pre-med hopefuls –– and will be going to Alabama for an emergency medicine fellowship later this year. His interest in this subspecialty stems from a penchant for critical care and working in the emergency department, which he regards as the “most fun.” In addition, Dr. MacDonald is going through the police academy that allows him to be on the S.W.A.T. team as a part-time, front-line physician, providing medical care to police officers and suspects.

I believe I speak for the majority of pre-meds when I pray that all of us can follow that same path as aspiring healers. But, as we know, the voyage to medical school itself is a daunting and lengthy affair. We are already at La Sierra University, so how do we undergrads march on from here? I asked Dr. MacDonald for some pre-med advice, especially some tips tailored towards factors affected by the COVID-19 pandemic, and he certainly delivered! For students applying to medical school, Dr. MacDonald strongly recommends being involved in community service, maintaining a high GPA, and achieving a decent MCAT score. Prior to med school matriculation, he wished he knew how to study as a med student because of the behemoth presentations of medical information to be mastered in a short period of time before setting foot on the clinical wards. Therefore, he suggested focusing on one to two main materials that are offered by the professors.
Last but not least, Dr. MacDonald’s final pearl to students pursuing an M.D. is to make sure they love the art and science of medicine because they have to live with this career choice for at least the next 30 years of their lives. And, while it is crucial to work and study diligently (though worth it in the long run, keep in mind that this may lead to sporadic phases of burnout), it is important to explore the world around you, appreciate nature, enjoy hobbies, hang out with friends, and to “have fun and be happy” throughout the four years of undergrad at La Sierra University.
— Ailinh Nguyen (Biomedical Sciences, Class of 2023)

